萬能抗體鎖提高抗體藥物對疾病區域選擇性以降低副作用
近年抗體藥已為臨床主流,然而抗體所辨認之抗原除了在疾病區表現外亦存在於正常組織,長期全身性中和抗原易產生嚴重副作用,如:類風濕性關節炎藥物Remicade可藉由中和關節炎區域的腫瘤壞死因子α (TNF-α)減緩發炎症狀,但TNF-α為重要免疫因子,長期全身性抑制下將降低患者免疫力,提升嚴重性感染風險(如肺結核)。因此如何提升抗體對疾病區抗原選擇性以降低副作用乃當務之急。本團隊開發萬能抗體鎖平台,以抗體Hinge結構作為抗體鎖,屏蔽抗體的抗原結合位,並藉由蛋白酶專一性受質胜肽連結形成前驅抗體,唯在蛋白酶過度表現疾病區,抗體鎖才能被移除,回復抗體原有結合力,提升抗體對疾病選擇性並降低副作用。目前已證實抗體鎖可屏蔽Remicade 269倍結合力,且經蛋白酶活化後其結合能力可完全恢復。抗體鎖可有效避免抗藥抗體中和pro-Remicade。在活體中更證實pro-Remicade選擇性活化於疾病區,並有效減緩類風濕性關節炎症狀;經由伺機性感染實驗發現,施打pro-Remicade小鼠組別存活率高於施打Remicade組別71%之多,證實pro-Remicade可有效改善Remicade副作用問題,成果在2019年被頂尖期刊PLoS Biol. 2019 Jun 13;17(6)刊登 IF=8.386 (13/189=6.8%),目前此技術平台專利已全球布局15個國家,獲得十個國家專利認證,完善的專利保護將加速其產業運用。抗體鎖平台可通用於各種單株抗體藥物,如類風濕性關節炎用藥(Remicade、Humira)、骨質疏鬆症用藥 (Prolia)、牛皮癬用藥(Stelara) 及癌症用藥 (Herceptin、Yervoy、Opdivo),皆可套用本抗體鎖以屏蔽抗體結合位,且抗體鎖可被蛋白酶選擇性活化並完全回復抗體功能,另外我們也建立以電腦結構模擬出抗體鎖屏蔽各式抗體的效率,可客製化產生各種前驅抗體,加速產業化效益。基於以上成果、抗體市場性與疾病的需求性,我們已利用抗體鎖平台成立創新研究服務公司積極進行產業推廣,相信抗體鎖可為抗體產業帶來更大的經濟效益。透過本抗體鎖,即可開發具有選擇性且低副作用的"前驅抗體藥物",對抗體產業帶來革命性的影響,並帶給病人更佳的生活品質與療效。
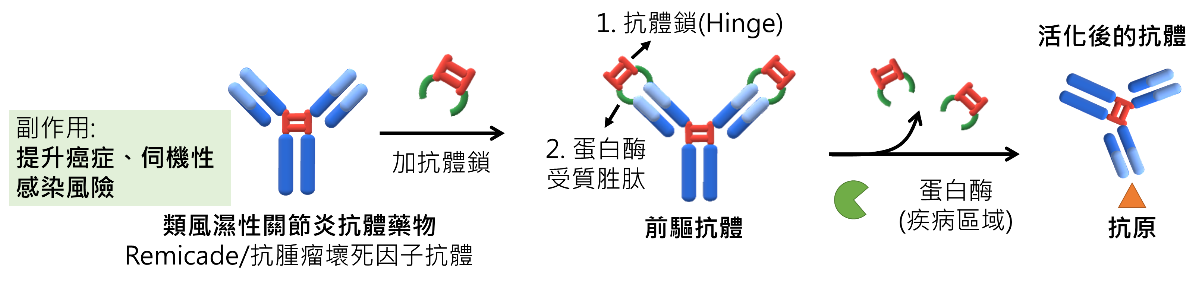
長期使用類風濕性關節炎抗體藥物Remicade將提升癌症及伺機性感染的風險,為提升抗體藥在疾病區選擇性以降低副作用,我們利用抗體自身Hinge結構作為抗體鎖,以蛋白酶受質胜肽連結抗體形成前驅抗體,唯有在蛋白酶過度表現疾病區才能回復抗體功能,增加抗體藥對疾病區選擇性,並降低副作用,將大大改善病人抗體用藥的生活品質。
本篇為高雄醫學大學2019年傑出論文及2019年月傑出論文6月份得獎文章,代表作者為高雄醫學大學生物醫學暨環境生物學系鄭添祿教授。
本校主要研究者之簡介: 鄭添祿 講座教授兼研發長
研究聯繫Email: tlcheng@kmu.edu.tw
期刊出處: PLOS Biology
期刊線上參閱網址: https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000286
Universal antibody lock can enhance the disease selectivity of antibody drugs to reduce side effects
Long term administration of therapeutic antibody (Ab) can lead to serious adverse effects. It will be a great business opportunity to reduce side effects by enhancing the selective targeting of Ab to disease region. We used hinge domain as Ab lock to link the Ab by protease substrate peptide, to generate a pro-Ab that will block the binding of Ab to the antigen. The Ab will be revived by specific protease which overexpressed in disease region, the selectivity of Abs to disease region will be increased and reduce side effects. Results showed the binding of pro-Remicade was 269.5-fold weaker than Remicade and completely restored after activation with protease. Compare to Remicade, Pro-Remicade provided equivalent serum half-life and therapeutic efficacy while minimizing the interference in immunity against Listeria infection. Moreover, patents have been filed in 15 countries. We expect the Ab lock for improving selective activation of Abs can improve the quality of life in patients and cause revolution of Ab drugs industry in the future.
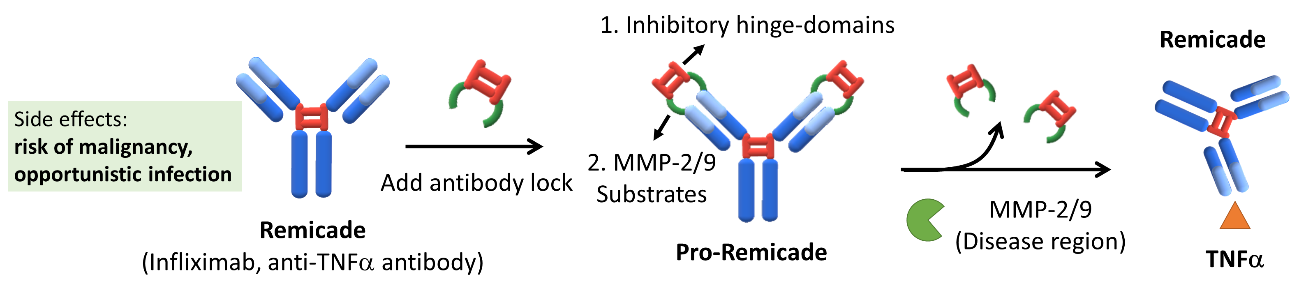
We used an autologous hinge as antibody lock to cover the antigen-binding site of Remicade by using MMP-2/9 substrate linker to generate pro-Remicade. Upon protease activation at the rheumatoid arthritis region, the antibody lock was released, and the pro-Remicade could specifically activate and neutralize TNFα at the disease site to inhibit rheumatoid arthritis progression.
Main researcher Intro.
Tian-Lu Cheng
Author Email: tlcheng@kmu.edu.tw
Paper cited from: PLOS Biology
Paper online https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000286
國內六家媒體:
【中時電子報】高醫大研發「萬能抗體鎖」商機百億美元 美日台藥廠洽授權
https://www.chinatimes.com/realtimenews/20190710001907-260410?chdtv
【聯合新聞網】高醫大萬能抗體鎖助減藥物副作用 申請國際專利
https://udn.com/news/story/7266/3920786
【中央社】高醫大萬能抗體鎖 獲多國專利
【經濟日報】高醫大「萬能抗體鎖」技術獨步全球 商機無限
https://money.udn.com/money/story/5724/3920726
【大紀元】獨一無二 高醫大「萬能抗體鎖」降低藥物副作用
【工商時報】高醫大研發「萬能抗體鎖」商機百億美元 美日台藥廠洽授權
海外二家媒體:
【THE CENTER FOR BIOSIMILARS】In Early Study, Researchers Modify Infliximab to Make It Safer, More Effective
【ScienceDaily】'Locking' an arthritis drug may be key to improving it
https://www.sciencedaily.com/releases/2019/06/190613143541.htm
基因交互作用大大影響胰臟癌病人對藥物的反應
胰臟癌是非常惡性的腫瘤,病人的五年存活率在8-10%左右。因為胰臟癌不易早期發現,只有20%左右的病人可以開刀治療,在轉移的病人,目前化療大多是以Gemcitabine組合的藥物當作第一線的治療,然而藥物的反應率低,所以胰臟癌病人的存活率在近20年並無明顯的改善。
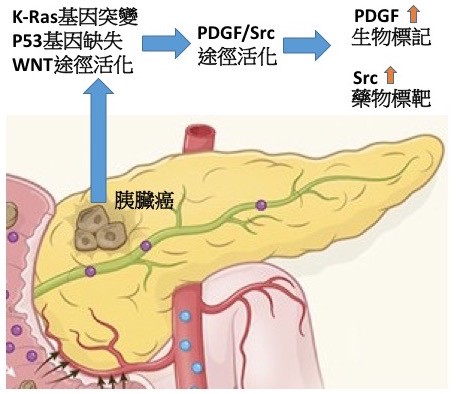
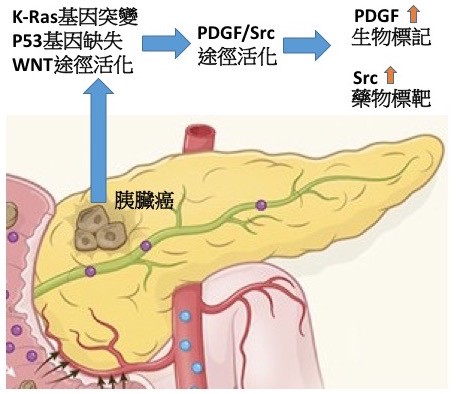
精準醫學是癌症治療上非常重要的一環,不同的胰臟癌組織存在不同的基因缺陷,這些基因異常可單獨或協同活化不同的訊息傳遞途徑,所以癌症病人對化學或標靶治療的反應性有很大的差別。如何藉由細胞實驗,動物模式及病人基因檢測找到藥物反應的生物標記(Biomarker)是基礎研究人員與臨床醫師的共同目標。在胰臟癌中,變異最高的兩個基因是K-ras與p53。然而除了這兩個基因外,常有第三個基因缺陷,本校洪文俊副校長領導的團隊發現WNT/β-catenin途徑的變異存在約20%的胰臟癌病人。團隊建立了基因轉殖鼠的動物模式,研究發現相較於只有K-ras與p53變異的基因轉殖鼠,具有第三個WNT/β-catenin途徑基因缺陷的老鼠會特異性的增加血小板衍生生長因子(PDGF)基因轉錄,進而產生大量的PDGF來刺激胰臟癌細胞與星狀細胞生長,快速促進胰臟癌惡化轉移。進一步,團隊與國家衛生研究院及國立成功大學醫學院合作,在胰臟癌病人的血液與腫瘤組織印證了臨床相關性。更重要的,藉由分子機制探討及藥物篩選,團隊發現PDGF途徑特異性活化下游的訊息傳遞分子Src,所以具有三個基因缺陷的老鼠對Src抑制劑特別敏感,顯示此類藥物對具有特定基因變異的胰臟癌病人可能有更顯著的治療效果。此外血液PDGF的含量也可以是當作篩選病人的生物標記。本研究建立了新穎的胰臟癌動物模式來探討變異基因之交互作用對胰臟癌惡化與轉移的影響,同時找到了一個血液生物標記可用於篩選適合於標靶治療的胰臟癌病人(如圖示),達到精準醫療的目的,相關研究成果發表於國際期刊Theranostics。
本篇為高雄醫學大學2019年傑出論文及2019年月傑出論文1月份得獎文章,代表作者為醫學院醫學研究所洪文俊教授。
基因交互作用大大影響胰臟癌病人對藥物的反應
胰臟癌是非常惡性的腫瘤,病人的五年存活率在8-10%左右。因為胰臟癌不易早期發現,只有20%左右的病人可以開刀治療,在轉移的病人,目前化療大多是以Gemcitabine組合的藥物當作第一線的治療,然而藥物的反應率低,所以胰臟癌病人的存活率在近20年並無明顯的改善。
精準醫學是癌症治療上非常重要的一環,不同的胰臟癌組織存在不同的基因缺陷,這些基因異常可單獨或協同活化不同的訊息傳遞途徑,所以癌症病人對化學或標靶治療的反應性有很大的差別。如何藉由細胞實驗,動物模式及病人基因檢測找到藥物反應的生物標記(Biomarker)是基礎研究人員與臨床醫師的共同目標。在胰臟癌中,變異最高的兩個基因是K-ras與p53。然而除了這兩個基因外,常有第三個基因缺陷,本校洪文俊副校長領導的團隊發現WNT/β-catenin途徑的變異存在約20%的胰臟癌病人。團隊建立了基因轉殖鼠的動物模式,研究發現相較於只有K-ras與p53變異的基因轉殖鼠,具有第三個WNT/β-catenin途徑基因缺陷的老鼠會特異性的增加血小板衍生生長因子(PDGF)基因轉錄,進而產生大量的PDGF來刺激胰臟癌細胞與星狀細胞生長,快速促進胰臟癌惡化轉移。進一步,團隊與國家衛生研究院及國立成功大學醫學院合作,在胰臟癌病人的血液與腫瘤組織印證了臨床相關性。更重要的,藉由分子機制探討及藥物篩選,團隊發現PDGF途徑特異性活化下游的訊息傳遞分子Src,所以具有三個基因缺陷的老鼠對Src抑制劑特別敏感,顯示此類藥物對具有特定基因變異的胰臟癌病人可能有更顯著的治療效果。此外血液PDGF的含量也可以是當作篩選病人的生物標記。本研究建立了新穎的胰臟癌動物模式來探討變異基因之交互作用對胰臟癌惡化與轉移的影響,同時找到了一個血液生物標記可用於篩選適合於標靶治療的胰臟癌病人(如圖示),達到精準醫療的目的,相關研究成果發表於國際期刊Theranostics。
本篇為高雄醫學大學2019年傑出論文及2019年月傑出論文1月份得獎文章,代表作者為醫學院醫學研究所洪文俊教授。